
Let us take a few steps back now and ask – why on Earth should anyone be interested in antibiotics at all?
Especially if one is not a student of medicine, a doctor, or at least a patient in need of a cure for their bacterial disease?
Take away antibiotics, and most sophisticated but routine medical procedures will collapse like a pack of cards. And as a matter of fact treatment failure is already common, with patients having complication or sometimes dying or spending many extra days in hospitals due to lack of effective antibiotics.
All that is truly terrifying. However, the purpose of what we are trying do in this book is not to try and scare you at all!
Fear and anxiety are not the best way forward while trying to find solutions – especially something as complex as:

With some rich insights we may finally begin to figure out what is the best way to slow down antibiotic resistance and keep antibiotics working:
- Where do antibiotics come from?
- How do they work?
- Why are they important?
- How many kinds of antibiotics are there?
- How does antibiotic resistance lower their
effectiveness?
And… if you are not already exhausted by that long list of questions – let us also ask how are they produced, distributed and consumed?
Ok. We will do this one at a time – step by step. First, we will start with the meaning of the term:


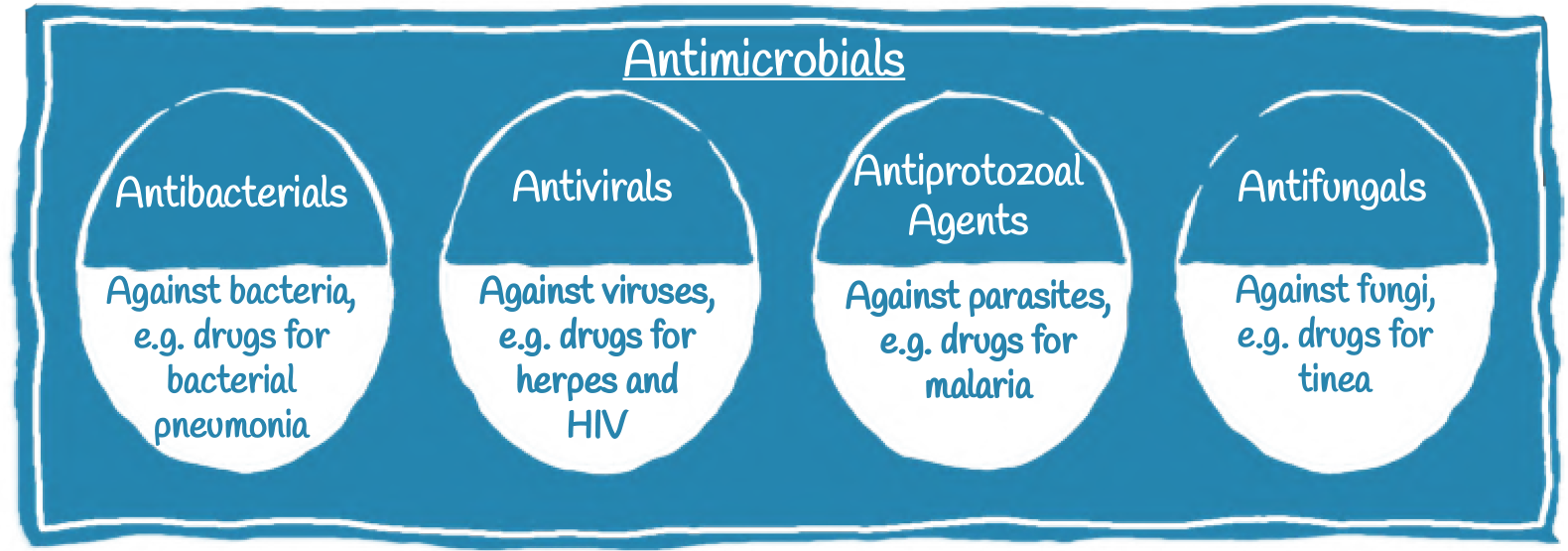
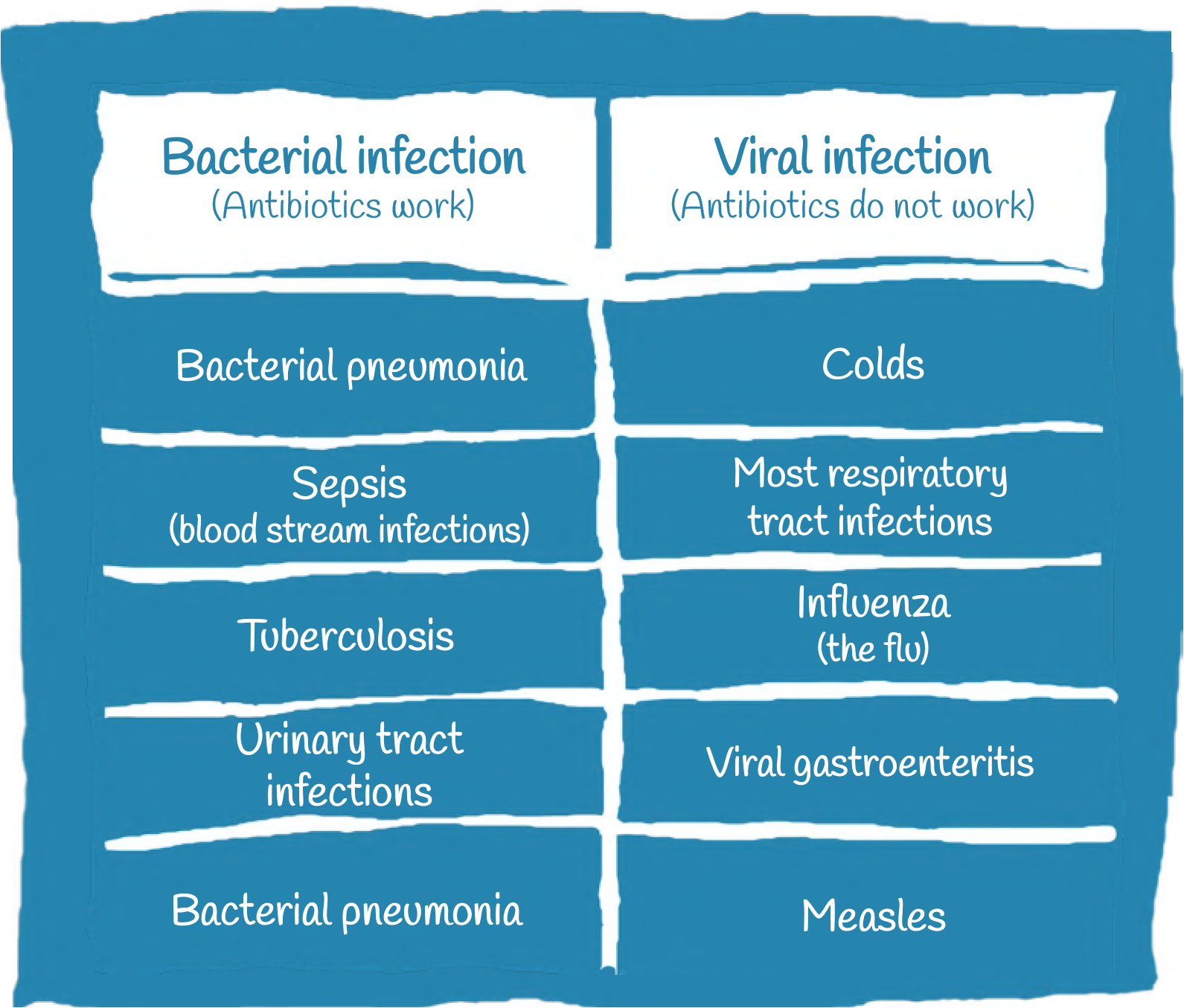
- Antimicrobials: Antimicrobials is a wider term that includes all agents that act against microorganisms, namely bacteria, fungi, virus, and protozoa.
- Antibacterials: Antibacterials act only on bacteria. This term encompasses all compounds that act against bacteria, including antibiotics.
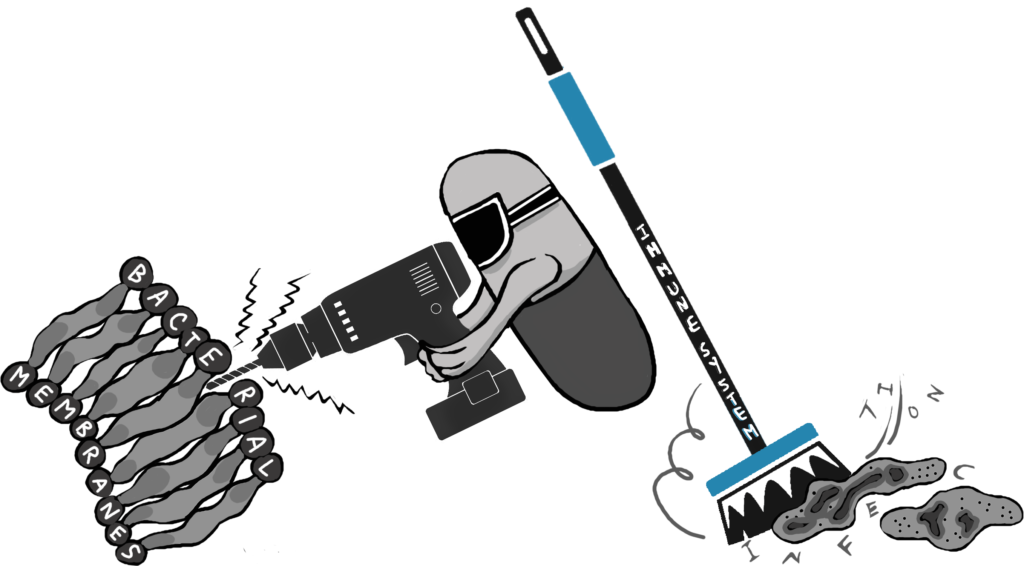
- Antibiotics: Antibiotics are produced naturally by microorganisms and kill or inhibit the growth of other microorganisms, mainly bacteria.
- Strictly speaking, antibiotics do not include agents that are produced by chemical or biochemical synthesis. However for simplicity, synthetic or semi-synthetic variants (such as quinolones) are usually included under the term antibiotics.
The discovery of antibiotics was one of the most significant medical achievements of the 20th century.
In the pre-antibiotic era of the early 1900s, people had no medicines against bacteria and as a result, human suffering was enormous. Even though the body’s disease-fighting immune system can often successfully fight off bacterial infections, sometimes the microbes are too strong.
For example,
• Before the advent of antibiotics, 90% of children with bacterial meningitis died. Among those children who lived, most had severe and lasting disabilities, from deafness to mental retardation.
• Throat infections due to a bacteria called streptococci was at times a fatal disease, and ear infections sometimes spread from the ear to the brain, causing severe problems.
• Tuberculosis, Typhoid fever, Gonorrhea are treated with antibiotics today. Imagine what would happen if they become untreatable.
Like all medicines, antibiotics have the potential to cause side effects. When antibiotics are necessary, the benefits far outweigh the risks, but when they are not needed, you are taking an unnecessary risk.
Up to 10% of people taking an antibiotic may experience these common side effects:
• stomach problems like diarrhoea, nausea and vomiting.
• fungal infections, which can affect the mouth (white patches will be visible) and in women can also occur in the vagina (causing itchiness, pain
and discharge).
Other less common side effects include:
• diarrhoea caused by an intestinal infection, which may be serious and require further investigation and treatment
• allergic reactions, such as hives (large, red, raised areas on the skin), fever and breathing problems.
• Antibiotics that affect a wide range of bacteria are called broad spectrum antibiotics (e.g., tetracycline).
• Antibiotics that affect only a few types of bacteria are called narrow spectrum antibiotics (e.g., benzyl penicillin.
Narrow spectrum antibiotics are more specific and only active against certain groups or strains of bacteria. Broad spectrum antibiotics instead inhibit a wider range of bacteria. Narrow spectrum antibiotics are preferred since their impact on other, non-disease causing bacteria are more limited.
Unfortunately broad spectrum antibiotics are used more often as it can be difficult for doctors to diagnose the correct bacteria in time or the knowledge about how to correctly treat an infection may be lacking. This is one of the reasons for the emergence of antibiotic resistance. We will find out exactly why soon.
