
Dealing with patients or members of the public constantly brings in various other factors into the actual practice of medicine. In other words, the story of medicine is a combination of findings from various natural sciences along with that of social sciences such as communication, psychology, sociology, anthropology and even political knowledge.
The anthropological approach
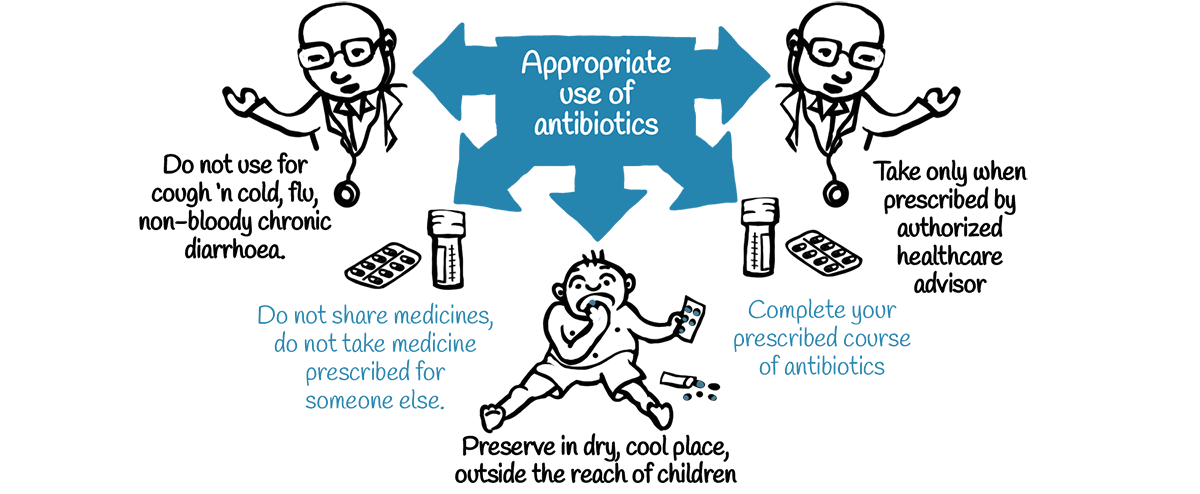
Much of antibiotic resistance, whether in the human or health sector, is driven by the ‘inappropriate’ use of these critical medicines – which in turn is the outcome of various powerful factors shaping prescription or health seeking behaviour. Without a good understanding of these myriad factors, ranging from medical science to anthropology, it will be difficult to design effective policies or interventions to tackle the problem.
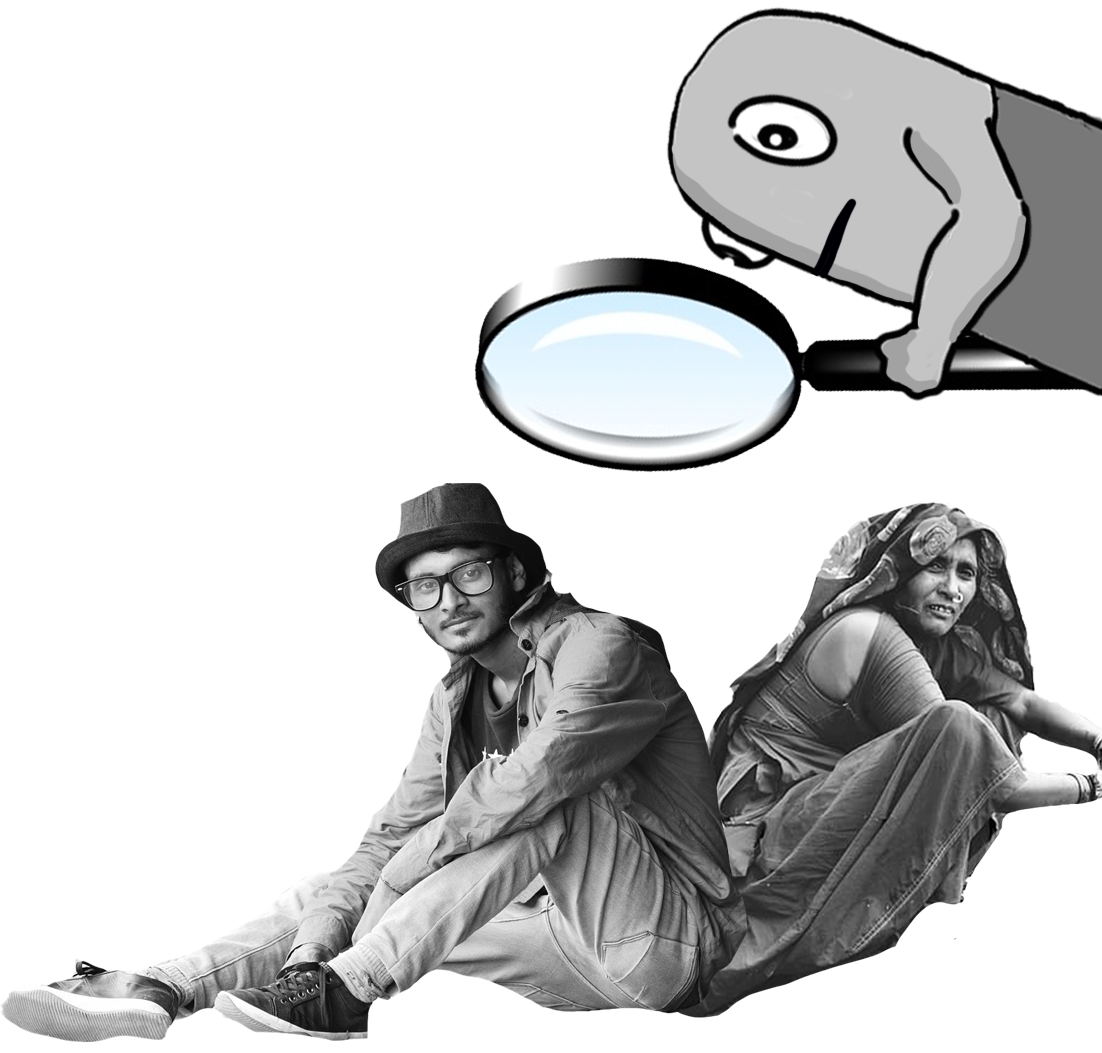
It cannot be assumed that a single conception of what ‘health’, ‘disease’ or ‘medicine’ mean – even if it is the most ‘rational’ and ‘evidence based’ – would be wholeheartedly accepted by the vast and diverse populations of the world. The infant, the young, the elderly, men, women, rich, poor, the indigenous, the urban or rural and those who come from different personal and social histories cannot be all put under the same petri dish to be examined under a lens with the hope of arriving at one general formula for intervention.
This means that there cannot be one common standard set of criteria to define what constitutes ‘good health’ imposed on this diversity of worldviews. What people choose to do with their bodies and how they look after them is closely related to the context, culture and traditions they come from.
The only way to work on anything to do with health and medicine then is with the full participation of communities and individuals in a patient, respectful and organic process to arrive at common goals and objectives through consensus.
A planetary perspective
While there has been recognition of the role of social, cultural and economic determinants that shape the health of all populations for quite some time now, there is also growing acknowledgment of planetary processes involved. As the Rockefeller Foundation-Lancet Commission on planetary health says in its 2015 report:
“Changes to the structure and function of the Earth’s natural systems are a growing threat to human health.Expect future substantial health effects from the degradation of Natures’ life support systems.”

Climate change is an obvious example of a phenomenon that, if not brought under control, can create conditions that bring the very existence of the human and other species itself into question. Mother Earth itself is sick today due to human actions over the last several centuries following the industrial revolution.
It is time to recognize that at the planetary level itself there is disease all around, all of which are intimately connected to the well-being of individual humans.
There are countless ways how ‘big picture’ phenomenon impacts each of us as individuals. Air, water and soil pollution, declining nutrient content of available food, growing population density of cities, loss of biodiversity, lack of occupational safety, loss of income and jobs due to economic crisis, increased mortality and morbidity due to conflict – these are all planetary level diseases which need to be addressed as an integral part of any national or global policy on health and medicine.
The implication of this planetary approach is very straightforward. The primary medicines all humans truly need are good nutrition, clean air, clean water, safe environments, ability to live with dignity and a peaceful social milieu.
It is only on this sound foundation that the problem of antimicrobial resistance will ultimately become truly manageable.
It is therefore imperative that we imbibe the lessons that the past and the present have taught us, to ensure that the journey of the antibiotic continues into the future!

