
The argument is correct, except that it turns out, for all this focus on the medicines themselves, there is another important driver behind the spread and emergence of antibiotic resistance. And this is none other than the high number of bacterial infections itself.

It has been found that wherever there is more infectious diseases due to bacteria, there is also greater prevalence of resistant infections. Therefore, the prevention or reduction of bacterial infectious diseases is very important to lowering antibiotic resistance.
Disease burden due to communicable diseases vs. GDP per capita, 2017
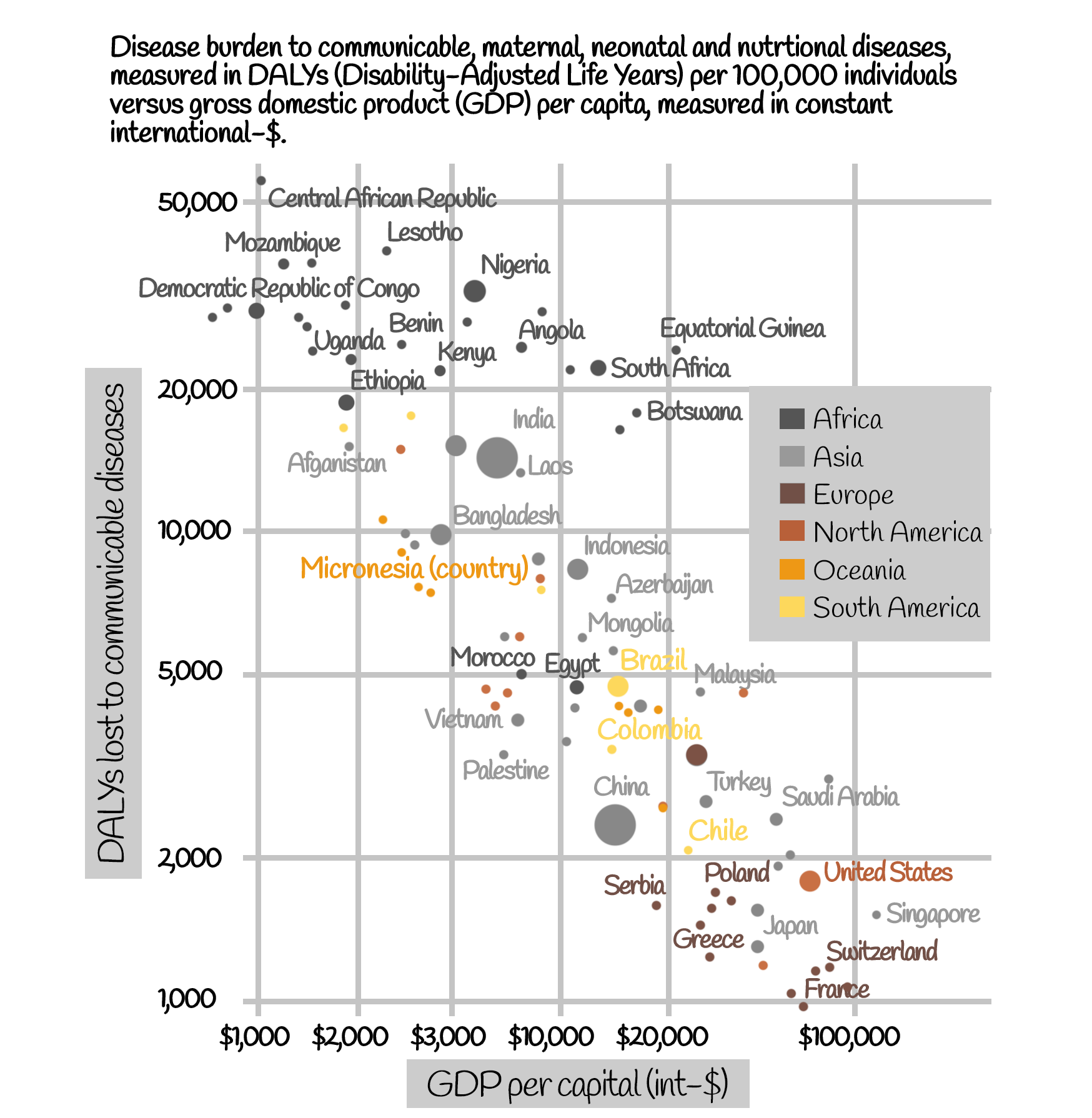
Source: Institute for Health Metrics and Evaluation, Data compiled from multiple sources by World Bank; ourworldindata.org/burden-of-disease/
Prevention and poverty
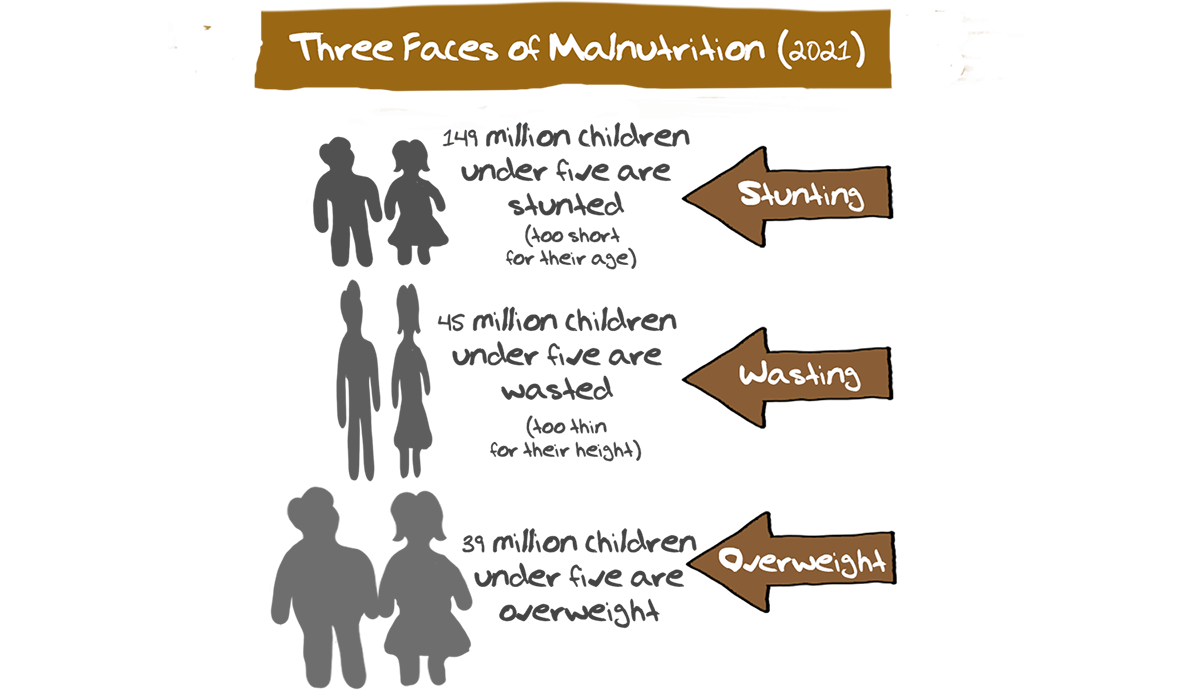
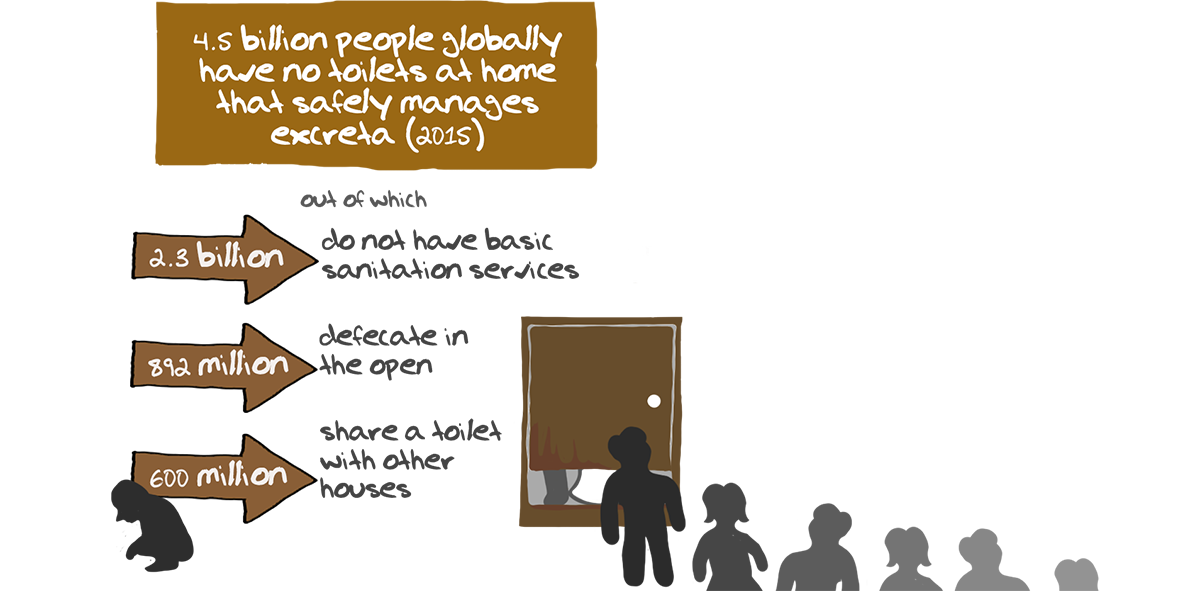
Prevention though is not as easy as it may sound. The drivers of infectious diseases are both diverse and numerous, including malnutrition, lack of safe drinking water, poor sanitation, pollution and lowered immunity of people due to other diseases.
One-third of the world’s population do not have a safe toilet; more than 660 million people do not have access to clean drinking water, and 1 in every 8 people currently defecates in the open.
People living in poverty, due to their circumstances, often engage in practices that drive antibiotic resistance such as irrational use and self-medication for themselves or their family and children. In fact, it may not be a coincidence, but many poor countries around the world are more susceptible to the causes and consequences of antibiotic resistance.
So, one of the important strategies towards tackling antibiotic resistance globally could be for richer parts of the world to provide poorer parts, with the material and technical resources needed to provide their citizens with sufficient food, sanitation and clean habitats. This will require not only stepping up of worldwide efforts at poverty alleviation but also ensuring a greater role for LMICs in global institutions and decision making bodies.

UHC and AMR
Given that tackling antibiotic resistance has been recognized as a challenge involving a wide range of sectors, attention in recent years has focused on implementing Universal Health Care (UHC).
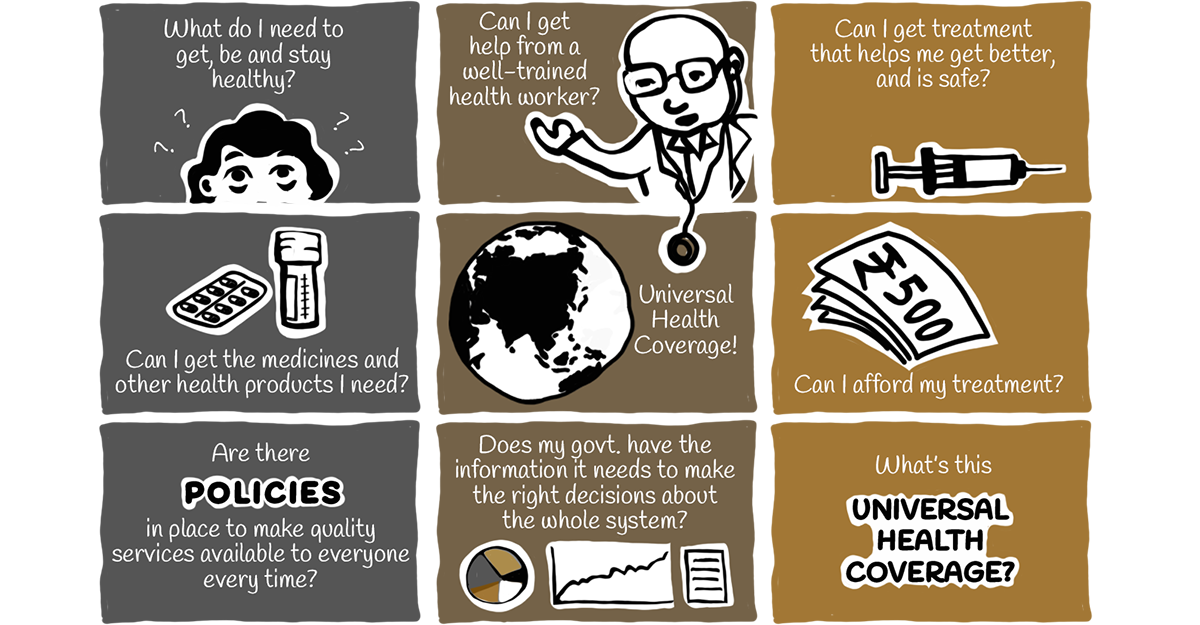
The WHO defines UHC as:
“All individuals and communities receive the health services they need without suffering financial hardship”.
In a good UHC system all citizens are provided the full spectrum of essential, quality health services, from health promotion to prevention, treatment, rehabilitation, and palliative care.
According to the WHO, at least half of the world’s population still does not have full coverage of essential health services, most of them living in Low and Middle Income Countries (LMIC).
While a UHC system, to be truly successful has to address AMR and related issues, strengthening health systems can contribute to tackling bacterial resistance.
Some of the benefits of UHC include:
• Greater breadth and depth in the population coverage of health services.
• Improved access to services like vaccination, preventative care and hygiene measures that lower the need for antimicrobials and thus slow the spread of AMR.
• More efficient and equitable financing to help close existing access gaps for treatable infections.
Health literacy
Another key resource needed to prevent bacterial infections is knowledge of health systems, medicine and diseases.
Quite often, people think that the field of medicine is so specialised or complicated that there is no point in trying to learn much about it themselves. As long as they have a good doctor or hospital to go to, everything will be all right.
This attitude of blind faith adopted by many patients leads to a situation that puts a lot of pressure on doctors to solve all the patient’s medical problems quickly. It becomes difficult for them to explain to patients that in reality, there are no easy solutions available.

If patients were more knowledgeable about the basics of health, medicine and disease, and less driven by anxiety and fear, this empowerment could enable patients to be contribute to their own health in partnership with medical professionals.
Health literacy of the population is critical to ensure success of any health intervention, whether it be avoiding disease or using medicines appropriately.
An alert and informed patient can help doctors do their job better and contribute to the overall health of the society by spreading the right message all around.


